Interview with Dr Surina Chibber My Locum Manager (MLM) Co-founder and Gemma Markham, Senior GP Commissioning and Development Manager for
NHS Derby and Derbyshire ICB.
Surina and Gemma shared their thoughts on why My Locum Manager was chosen for Derby and Derbyshire, how the project is going, and the challenges facing ICBs in encouraging adoption and utilisation across practices and clinicians.
Derby and Derbyshire ICS and MLM’s Beginnings
To start, Gemma shared some background information on Derby and Derbyshire ICB and the ground they cover. “Derby and Derbyshire ICB was formed in July this year,” she said. “We’ve got 114 GP practices which have grouped into 17 primary care networks (PCNs), covering a population of about 1.7 million and the demand for primary care is going through the roof. We’re delivering about 90,000 additional appointments a month and MLM has been an absolute asset to our primary care workforce.”
Surina picked up here: “I’m a GP by background, I’ve worked at a frontline general practice for many years now. I can see things from a GP perspective but also from a patient viewpoint – I’m a mum of two and I need to access GP services in my personal life aside from work.
“There has been a huge challenge for GPs up and down the country – recruitment numbers have gone down steadily over the last few years and the pressure on general practices to keep up with demand is increasing year on year.”
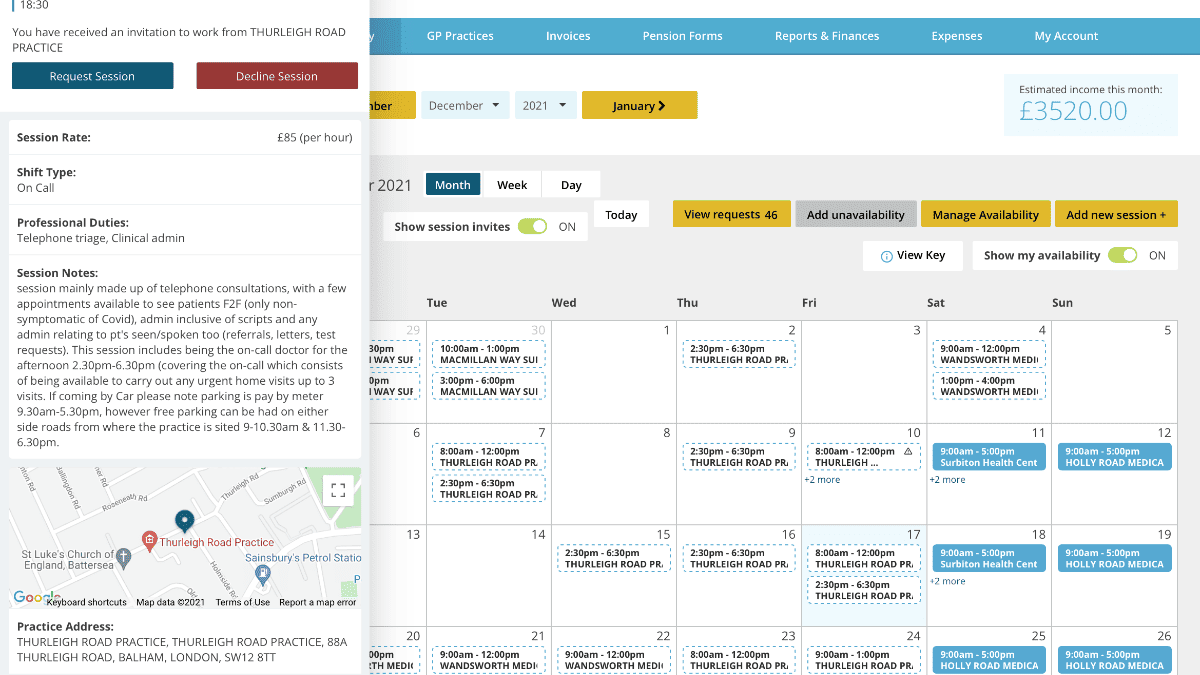
Surina explained how MLM was set up in 2016 alongside a fellow GP, and originally started as a membership community for GPs who wanted to work flexibly as locum doctors. “The main difference with our system was that it enabled GPs to build connections with local practices to manage their diaries,” Surina explained. “They could work around their childcare or other commitments, and it really formed a bond of regular working within their area.
“Fast forward two years and the flexible pools initiative was launched by NHS England and the idea behind the launch was supporting GPs and other healthcare staff to work flexibly across the area using digital solutions adopted across their ICB. The ultimate goal of the initiative is to meet more demand in practices with people who are familiar with the patients and have experience in the local area.
Navigating the workforce crisis without compromising patient care quality
“Patient care is always going to be at the centre of the way ICBs want to deliver care and I think that’s what attracted us to Derbyshire ICB,” said Surina.
“When we met them there was a long procurement exercise of their flexible pools. They were really thinking about wanting practices to have continuity with the GPs and other staff they employ. From our side, we want to have an environment where we can recruit and retain our GPs.”
Surina highlighted how the ICB had done a lot of research and looked at what practices wanted in terms of the stability of workforce.
“They were also thinking more about how to support their GPs and other staff to work flexibly around their commitments, making it more attractive for them to stay in primary care, which I really admired,” shared Surina. “With MLM, we wanted to provide a digital platform where they could actually access substantive posts as well – maybe they want to work as locum self-employed GPs for a time and build relationships with practices. That helps improve outcomes with patients too because you’re getting locally knowledgeable GPs that know the pathways, the protocols, the patient population that they’re looking after.”
She added: “MLM is the opposite of an agency model, it supports practice managers in building relationships with the self-employed GPs and allows them to invite the right GPs back time, and time again. Essentially, Derbyshire wanted a solution that secures continuity for their patients and practices whilst offering flexible ways of working for their primary care staff.”
“Something that attracted the ICB to MLM was their ethos around looking after staff,” Gemma noted. “Ultimately, doctors are patients too,” she said. “MLM taking care of staff’s wellbeing helps them to be healthy and means they can deliver their job well.”
A collaborative approach was taken with Derby and Derbyshire ICB, Surina explained. “Gemma and her team are really engaged with stakeholders,” she said. “They’ve got their GP Task Force in place and lots of other stakeholders to include the voice of practices and the voice of GPs – it’s allowed us as an organisation to be truly flexible in terms of planning for any upcoming needs and how we will work together to deliver it. Who is going to see that patient, and how are those staff members going to be accessed? How are they going to be presented with the right type of onboarding so they can deliver the care they are supposed to deliver? Do they know what referral pathways there are so that they can help the patient? It’s important to be mindful of simple things like whether or not they know what clinical systems are being used in the area.”
Ultimately, she continued, “I think the reason it worked so well is the collaborative approach with everyone involved working as one team sharing the same vision for the outcome, and continuing to adapt the solution so it best fits the needs of practices.
Gemma added: “The locums with MLM get access to any content that our GP Task Force offers to the wider primary care community, so people are working together in different ways.”
Challenges for utilisation and engagement of flexible pool solutions for ICSs
One of the main things about utilisation is whether the ICB is organised and engaged, Surina noted. “With Derbyshire, it has worked so well because they’re just on it with regards to getting stakeholders involved, helping to circulate comms, and having good relationships with practices. We’ve got a really good locum population across the area that we’ve also worked together to engage.”
She added: “That collaborative and one-voice approach has been really useful, and I think that’s also true of having regular feedback. Gemma and I will meet regularly, or we’ll be sending data across to each other which we can analyse. For example, we might spot an onboarding plateau and realise that we need to send out more comms about that.”
Looking at winter pressures, Surina noted that it is important to consider the marketing and engagement work that may be needed. “The cycle is ongoing,” she said, “and I think with to best utilise the software, you need an ongoing cycle to help capture practices when they’ve got the need. Initially, some of the practices were fully staffed and didn’t feel the need of joining but because we continued engaging with them, they can access our support when they have a sudden need. That ongoing relationship meant that we were able to just continue the onboarding cycle and treat it like a continuum of a service.”
A consideration for the future to maximise utilisation of the solution is to ensure that practice managers, as well as GPs, have a system that is easy to use and slots into other systems used within the ICB, Surina added. As part of this, MLM has worked on an integration with TeamNet which is “present in 70 per cent of practices” and manages workforce intranet and communication, intending to alleviate the need to log into different systems by allowing managers to use the MLM/TeamNet system for their workforce tasks as well.
At this point, Gemma entered the conversation to highlight some of the challenges that primary care is facing around workforce pressure. “We’re seeing people leave that maybe wouldn’t have left,” she commented. “There’s a lot of movement around practices because it’s becoming a competitive market with the current number of vacancies.”
Picking up on Surina’s point about making systems easily accessible, Gemma said: “That is absolutely essential for the way that primary care is working now. Staff haven’t got the time to shop around or ring up when they need a shift filling that same day. It’s always going to be difficult to fill those, but with MLM it’s easier than it ever has been and that’s what we need to be offering to our practices.”
“We hope the combination on offer in the ICB will make being a locum in Derbyshire really attractive,” she said. “MLM is filling in the gaps without all those challenges that come with using an agency.”
With regards to setting practice managers up on the system, Surina said: “When we first launched, our training model was a session for practice managers once a week. They could log on and through Microsoft Teams where they could complete their training. Later, we found out that by the end of the week, practice managers were so swamped that they couldn’t attend. So, we’ve shifted to on-demand booking and pre-recorded sessions which has helped to increase the number of practice managers trained to use the system.”
Now, she said, they have an implementation consultant who builds relationships with local practices and can offer flexibility for practice managers. “That’s been key to utilisation as well, to make sure that we understand that whilst managers do need this system, their time is very limited. So we need to work around them and their availability to get them trained up on the system and ready to go.”
Challenges around clinician engagement
“We’ve always sought to do it differently,” said Surina. “From the start, we built a membership platform which was based on delivering all the tools a GP needed to work how and when they wanted. It was about supporting them to work locally and build relationships with practice managers so they can become that practice’s go-to locum and could cover ad hoc shifts. Maternity locums and long-term locums can then develop those relationships to the point where they want to take on a permanent role.”
The vision is for locums to feel that they have been able to get a feel for different places and build up their experience, she said, and this has been supported through additional continued professional development, training, webinars, and community support. “We help to address the questions and challenges that they face, and that has become the foundation for our platform and attracted thousands of GPs to join.”
Once they were engaged into joining, Surina continued, it was about communicating to locums that they could source work through this platform as well as finding work from other sources. “You can add all the types of roles you’re doing because we can support portfolio working as well,” she said. “I think that was key to engaging clinicians. The market tends to dictate that you should make it all about the highest rate that’s on offer, but we did the opposite. We made it about the people. This is their livelihood; we’re here to help them build connections locally and get a sustainable income. We help them build relationships with practice managers so that they can deliver fantastic patient care and get support. Through those relationships, you know where to go for help if it’s needed.”
Success from the ICS point of view: establishing MLM as the flexible pools provider in the area
“It’s so much more than just filling the shifts,” said Gemma. “It’s about getting the locums to feel like they are part of our workforce, they should be just as valued as a partner that has been in the practice for 20 years. That’s what success would look like to us.”
The more shifts they fill, the more appointments they can deliver, but Gemma highlighted the importance of valuing workforce wellbeing. “Success is a happy workforce, and locums telling their friends that Derbyshire is a really nice supportive place to work.”
“It would be great if we could start attracting people to work here. Derbyshire is so diverse and MLM can support somebody to get a taste for what type of practice they want to work in.”
On MLM being approved for the NHS flexible pools framework
“This new framework has just been launched and I’m so proud to say we are part of that initiative,” said Surina. “We worked really hard to achieve that. We went through a really tough procurement process to go on that bid.” The next step with regards to the framework is to “really step up with meeting the challenges of primary care work like delivering workforce and meeting patient demand.”
Surina added: “It’s also allowing us to put the clinicians and the practice managers at the centre and focus on their well-being, as Gemma mentioned. With all the other aspects that we offer like the continued professional development training, I think it’s going to be a very exciting time.
“The first framework was a great ‘dip your toe in the water’ test. The results we found with the Derby/Derbyshire ICB and even the feedback from NHSE in what we’re doing has been incredibly positive so we can’t wait to expand that and just do more.”
What is in store for the future?
“Number one on my to-do list with Derbyshire is ramping up engagement for winter pressures,” said Surina, “and also looking at rolling out other staff types across the area. When you’re working in a practice, the workload and pressure has really increased across all staff, not just GPs. It affects reception staff, admin staff, and practice managers too. We’re constantly looking at new ways to help with that.
“I would say the project has gone really well and I really value the support from the ICB. There have been challenges along the way, but I think half of the time it’s actually nothing to do with practices or anything else, it’s just the landscape of primary care and COVID.”
Looking to the future, Surina said: “Our average shift fill rate is above 90 per cent – that’s great. But we’re here for the long-term with the ICB, and we share their vision of having a truly sustainable workforce. That isn’t just about the self-employed cohort, it’s about working with the permanently employed one as well. You need them for stability in the practices. Our next goal is to fully embed for winter pressures, remote consultations, and then the integration I mentioned earlier with TeamNet which will allow practice managers to manage all aspects of HR along with rotas for their permanent and self-employed staff in tandem. That will mean that they can cover workforce gaps much more efficiently and effectively.”
Gemma agreed. “A practice manager is so busy,” she said. “It will make it so much easier for them if they can have someone come in and use TeamNet to find all the information they need about how that practice is going to work, which will be so helpful for both sides.”
Thank you to HTN for the interview write-up.

